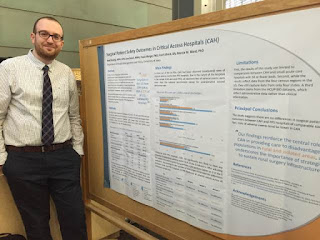
University of Iowa Quality Improvement Symposium Poster Presentation
By: Nabil Natafgi
PhD student, Nabil Natafgi, recently presented a poster at the fourth annual University of Iowa Quality Improvement Symposium. Background information and findings of the study presented in the poster are as follows:
PhD student, Nabil Natafgi, recently presented a poster at the fourth annual University of Iowa Quality Improvement Symposium. Background information and findings of the study presented in the poster are as follows:
Surgical Patient Safety Outcomes in Critical Access Hospitals: How Do
They Compare?
Nabil
Natafgi, MPH; Jure Baloh, MHA; Paula Weigel, PhD; Fred Ullrich ,BS; Marcia M.
Ward, PhD
Research Objective: Critical
Access Hospital (CAH) are the predominant type of hospitals operating in small and isolated rural areas, constituting
approximately 27% of all community hospitals in the US. The intent of CAH designation is to reduce
financial vulnerability of rural hospitals by providing a payment system based on cost, as opposed to prospective
payment system (PPS) – the predominant reimbursement model for larger urban-centered
hospitals. Such financial incentives are believed to improve access to healthcare by keeping
essential services in rural communities. This study aims to examine whether CAHs perform better than, the
same as, or worse than PPS hospitals on measures of quality.
Study Design: The Healthcare
Cost and Utilization Project State Inpatient Databases and American Hospital Association annual survey data were
used for analyses. Outcome measures included six bivariate indicators of adverse events of
surgical care developed from the Agency for Healthcare Research and Quality’s Patient Safety
Indicators (PSIs). Multiple logistic regression models were developed to examine the relationship between
hospital adverse events and CAH status. Population Studied: A total of 35,674
discharges from 136 nonfederal general hospitals with fewer than 50 beds were included in the analyses: 14,296
from 100 CAHs and 21,378 from 36 PPS hospitals.
Principal Findings: Compared to
PPS hospitals, CAHs are significantly less likely to have any observed (unadjusted) adverse event on four of the six
indicators. After adjusting for patient mix and hospital characteristics, CAHs perform better on three
of the six indicators. PPS hospitals were 7.7 times more likely to have any perioperative hemorrhage or
hematoma event compared to CAH hospitals with similar patient mixes, accreditation and system
membership status, and RN staffing ratios (P < 0.001). PPS hospitals were 4.3 times more likely to have
any perioperative pulmonary embolism or deep vein thrombosis event compared to CAH hospitals (P =
0.002), and 9.1 times more likely to have any postoperative sepsis case compared to CAHs with
comparable characteristics (P = 0.010). Accounting for the number of discharges eliminated the
differences between CAHs and PPS hospitals in the likelihood of adverse events across all indicators
except one. Patients were 6.3 times more likely to experience a perioperative hemorrhage or
hematoma event in PPS hospitals than in CAHs after adjusting for patient mix, hospital characteristics, and
number of discharges (P = 0.005).
Conclusions: The study suggests there are no differences in
surgical patient safety outcomes between CAHs and PPS hospitals of comparable size.
Implications for Policy or Practice: This study has considerable policy relevance in light of recent research showing conflicting conclusions about
quality of care in CAHs, and because health care reimbursement is increasingly shifting to
payment for reported outcomes and quality improvement efforts. The findings reinforce the central role of CAHs
in providing care to disadvantaged populations in rural and isolated areas, and underscore the importance of
strategies to sustain rural surgery infrastructure.
Full-text
available at: Natafgi, N., Baloh, J., Weigel, P., Ullrich, F. and Ward, M. M.
(2016), Surgical Patient Safety Outcomes in Critical Access Hospitals: How Do
They Compare?. The Journal of Rural
Health. doi: 10.1111/jrh.12176


Comments
Post a Comment